
PDA BEHAVIOUR INTENSITY AND PREVALANCE AT DIFFERENT THRESHOLDS.
NOTES ON WRITING THIS BLOG POST.
This blog post has been written over a course of the last few of months. It particular in the last several of weeks, I have added substantial amount of more detail to the piece than was originally intended. I stopped drafting this piece after around 5000 words plus references. Upon reading Soppitt (2021), I reflected on it and how I could include Wing et al (2011) diagnostic threshold in the diagram. Vitally, how Wing et al (2011) diagnostic threshold compares to the two thresholds above and below it. Additionally, adding questions that one can use to rank PDA diagnostic thresholds has forced me to re-evaluate some of my original justifications for how I ranked each threshold. It has led to me doing further analysis of some thresholds and more reflection. Presently, there is about 9200 words plus references.
This is a good thing; it shows I am critically engaging with the PDA source material and not resting on my laurels. I am making myself “work” to adequately justify my placing of each PDA diagnostic threshold discussed (as I should be doing). It also means there may be some slight contradictions, between my initial work in the draft, and the more recent reflections. If there are contradictions present, it most likely because I have not edited it out in proof reading, it would be best to double check with me, what I mean before latching onto it to critique my work.
PURPOSE OF THIS DIAGRAM.
It displays how different interpretations of PDA are defined by the diagnostic thresholds and their associated estimated prevalence of PDA. The scales on the graph do not have any established quantitative figures attached and is my best guess to show how they related to each other in a way that lay persons can easily understand. This image is only a model to something that is complex and in flux over time and throughout a person’s lifespan. Some might convert this image into a 3D one, with separate axes for intensity of demand avoidance behaviour and frequency of demand avoidance behaviour.
By “Demand Avoidant” Behaviours, I am going to say those associated to core 5 PDA traits, which I consider to be:
- Comfortable in role play and pretending.
- Continues to resist and avoid ordinary demands of life.
- Lability of mood, impulsive, led by need to control.
- Obsessive behaviour.
- Strategies of avoidance are essentially socially manipulative.
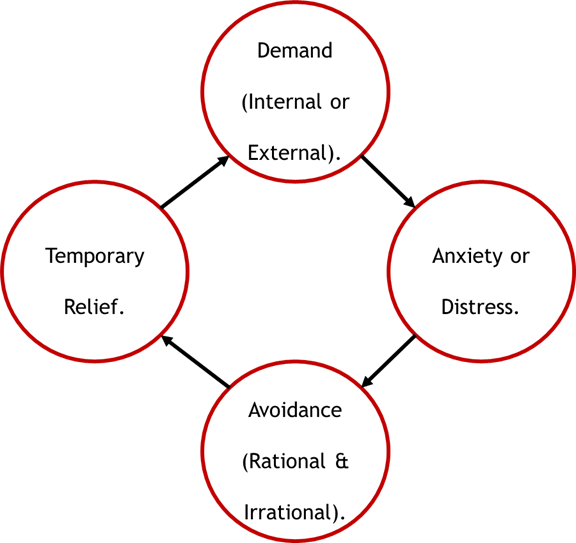
These 5 traits are all viewed as anxiety based restricted and repetitive behaviours and interests (RRBIs), which we know are not represented in diagnostic criteria, as anxiety is not a core feature of autism (Egan et al, 2019; Gould and Ashton-Smith, 2011; Woods, 2019b; Woods, 2020a). That all diagnosis thresholds should be based on these traits being present in a person and I in some capacity the demand avoidance should represent the below Demand Management Cycle (I will explain this more detail later in the blog):
This is important as autistic anxiety is often caused by aversive experiences (Pellicano, 2020), and that autistic persons have PTSD symptoms tend to be made worse with more trauma they receive (Rumball et al, 2021). Modern PDA understandings involve a transactional account (Fidler and Christie, 2019; Green et al, 2018; Milton, 2017), it means that how PDA presents in a person is somewhat dependent on how their environment (including other people) are interacting with the person. Some clinical accounts of PDA highlight persons transitioning into PDA (Newson, 1989; 1999; Newson et al, 2003; Wing, 2002; Wing et al, 2011). A few studies show PDA behaviours decreasing as Children & Young People (CYP) develop (Doyle et al, 2020; Newson et al, 2003; Woods, 2020a). The point is that a person will over the course of their life and in different situations move around the PDA Behaviour Intensity and Prevalence at Different Thresholds diagram and across diagnostic thresholds.
I accept that others may disagree with the interpretations and how I portray PDA here. This is an important point of the diagram, to show there are different conceptualisations of PDA and that can have major ramifications when interpreting research results.
Finally, I need to acknowledge that Professor Peter Kinderman suggested focusing on the management of demands, rather than their avoidance.
DIAGNOSTIC THRESHOLDS.
I will start by establishing the two extremes in diagnostic thresholds and interpretations in the PDA literature, moving down in diagnostic thresholds. As part of this I will explain how I made my decisions, what criteria have I applied:
There is only one diagnostic threshold that answer’s yes to all the five questions, which I believe is the strictest diagnostic threshold for PDA in the literature. The other five diagnostic thresholds mainly meet at least one these criteria, the only exception is the lowest diagnostic threshold, which answers no to all these criteria. I have not discussed these criteria as a checklist in each entry, but the readers should see if, and how each diagnostic threshold conforms to each of the criteria, or not. I have also used other information where possible to justify placing of each diagnostic threshold, such as predicted prevalence rates.
Table 1: Compulsory features that must be present for various PDA diagnostic thresholds.
| Features need to be compulsory. | DSM-5 OCD. | Eaton and Weaver (2020). | EDA-Q Threshold. | Gillberg et al (2015). | Newson et al (2003). | Wing et al (2011). |
| Demand avoidance ne Pervasive? | No. | Yes. | No. | No. | Yes. | Yes. |
| Demand avoidance from early infancy? | No. | Yes. | No. | No. | No. | No. |
| Person is autistic? | No. | Yes. | No. | No. | No. | Yes |
| Core 5 diagnostic traits present? | Yes. | Yes. | No. | No. | No. | No. |
| Coding issues present? | No. | Yes. | No. | Yes. | Yes. | Unsure. |
While Newson presented a behaviour profile for PDA, she did not require a person to display all the features or all the traits to receive a PDA diagnosis. She expressed in her article’s supplementary notes:
“Clearly no child will show all the behavioural examples listed, any more than all autistic children show the whole repertoire of autistic behaviours; but every child with clear-cut PDA will manifest the overall complex pattern, not merely one or two features.”
This is reflected in the statistics of many features represented in her cohort. Here are some statistics for features indicative of trauma and high arousal levels, which are only seen in around two thirds of her cohort:
Surface Sociability features: Aggression to others (no sex differences) – 68%.
Extreme outbursts or panic attacks – 60%.
Lability of mood features: Extreme lability of mood – 68% of CYP, of these 30% CYP including switching from love to hate.
It should be clear these features were not universal among persons with PDA in Newson et al (2003) database.
Considering some PDA traits are no longer required for a diagnosis due to being too common in autistic persons to be useful in identifying PDA (O’Nions et al, 2016). Additionally, traits are predicted to be removed as our understanding with PDA develops (Christie et al, 2012). The purpose of a PDA diagnosis is to assist persons and those around them, primarily through providing a better understanding of their actions, and to underpin support packages (Christie, 2007; Newson et al, 2003). It is reasonable to not to require all PDA traits to be present when diagnosing PDA. Due to this the 5 core PDA traits should be viewed as a guideline, and do not need to present in all persons with PDA. This has implications for the table of questions one could use to assess the severity of diagnostic threshold, it means that the question on all 5 core PDA traits being present is not necessarily a useful indicator and misses the point behind a PDA diagnosis. I am unsure if the other 4 questions are useful for probing different diagnostic thresholds, they do give some indicator in how the various PDA diagnostic thresholds are different/ like each other.
I will start by describing what I consider to be the lowest diagnostic threshold, Gillberg et al (2015).
Gillberg et al (2015).
The diagnostic threshold is wording as:
“Individuals with a Total PDA score of 5 or more were—based on clinical experience, not on systematic evidence—considered High-scorers, suggesting that in clinical practice they would have been given a diagnosis of PDA. “Classic PDA” was defined as Total PDA score of 5 or more and including the presence of socially manipulative or shocking behaviour to avoid demands.” (Gillberg et al, 2015, p981).
This is showing PDA features on 5 out of 17 (15 reported and two questions that assess for Speech Delay trait). A problem is that this threshold does not require the 5 core traits to be present, and it is possible that a person may meet threshold for “Classic PDA”, without having all 5 traits present, by scoring on questions that do not assess one or more of the core traits (Gillberg et al, 2015). Crucially, not requiring socially manipulative behaviour to be universal for a “Classic PDA” diagnosis, is a lower threshold than Elizabeth Newson, as she reported socially manipulative behaviour to be universal among her case studies (Newson et al, 2003). Gillberg et al (2015) reported they had a prevalence rate for PDA of 18% of autistic persons, and that only 1 out of 9 cases presented full PDA into adulthood. Worth noting that Newson also saw a decrease in negative aspects of PDA being observed by caregivers, as it seems that CYP with PDA could be taught right from wrong (from whose perspective?) (Newson et al, 2003).
Gillberg et al (2015) argue that PDA is potentially relatively common, seen in up to 3% – 5% of some populations. This mirrors previous comments by Christopher Gillberg that PDA is a common phenomenon, suggesting many predicted populations and questions if PDA is a new type of mental disorder (2014). While I admit I think PDA is a new type of mental disorder, if you wish to read more, please see this link below:
https://thepsychologist.bps.org.uk/pda-new-type-disorder
Next, I present what I consider to be the highest PDA diagnostic threshold.
Eaton and Weaver (2020).
Eaton and Weaver (2020) have presented findings from their case files of diagnosing PDA only in autistic persons and they use an informal algorithm of these definitions:
“demand avoidance has been present since early infancy and presented across different contexts and time“
“features of the child’s demand avoidance were noted in the child during the assessment process“
“avoidance was pervasive and often seemed illogical or perverse (e.g. the child maybe unable to eat when hungry)“
“avoidance was not limited to a specific activity (or activities) or activities in a specific context (e.g. school)” (Eaton and Weaver, 2020, p37).
A note, that these definitions are from non-autistic observer’s perspectives, so if the demand avoidance is perverse or illogical, or rational is not from autistic perspectives. Although, the clinic argues the view that RDA is different, as it is has an identifiable cause.
I also have concerns on requiring a person, even a CYP to display what is recognised as distress behaviour during an assessment to receive a PDA diagnosis. Eaton and Weaver (2020) note that anxiety appears to be driving CYP’s avoidance and discuss strategies clinicians required to be deployed to engage the CYP as part of the assessment. Moreover, discuss in detail how demand avoidance in CYP with PDA impacts the scoring on an autism diagnostic tool. One must acknowledge the skill displayed by Eaton and Weaver’s colleagues as part of the assessment process when faced with physical acts and sometimes threats of violent behaviour. However, one does not to recognise that it is requiring a CYP to display demand avoidance as part of the assessment process, ignores how an CYP can camouflage as part of the assessment.
More importantly, I fail to see how it is ethical to need a CYP to be displaying distress behaviours to receive a PDA diagnosis. The implication is that CYP has be distressed by the assessment process and therefore is made distressed by the assessing clinicians to express demand avoidance. This outlook is in line with transactional accounts of PDA, and does not follow suggested guidelines of managing PDA, of matching demands to a child’s tolerance levels (Christie et al, 2012; Fidler and Christie, 2019).
These definitions for demand avoidance are based on definitions of Pervasive, Developmental and Disorder used by Phil Christie, as PDA is conceptualised as a Pervasive Developmental Disorder, not an autism spectrum disorder by Newson (Newson, 1983; Newson et al, 2003). How PDA is conceptualised as part of the autism spectrum, is because people conflated the Pervasive Developmental Disorders diagnostic grouping with the Autism Spectrum (Christie, 2007; Christie et al, 2012). These are two different things, the autism spectrum is smaller than the Pervasive Developmental Disorders, as it only contains Asperger’s Syndrome (High Functioning Autism), Autistic Syndrome (Kanner’s Autism), and Pervasive Developmental Disorder- Not Otherwise Specified (PPD-NOS) (Christie et al, 2012; Green et al, 2018). That autism spectrum is based on the Triad of Impairment (Milton, 2017). While the definitions for Pervasive Developmental Disorders are:
“Pervasive suggests that the effects can be seen in all a child’s development.
Developmental means that the disorder is present at birth, gradually becoming apparent during the course of development.
Disorder implies more than straightforward delay.” (Christie 2019).
One would note that Eaton and Weaver definitions require PDA to be from early infancy and this contradicts other research and clinical opinion, which I will discuss next to establish that is of Wing et al (2011).
Wing et al (2011).
Wing et al (2011) article was authored by Wing, Gould and Gillberg. In terms in which I am using the article to mainly refer to the views of Wing and Gould. This is mainly as Christopher Gillberg has expressed his views on PDA separately to Wing and Gould, it appears to significantly different to latter. Gillberg’s views on PDA are discussed in more detail in the section for Gillberg et al (2015).
The views of Wing et al (2011) view PDA to be a form of autism, and so it is unlikely the author’s diagnosed PDA in non-autistic persons. In my view, the views written in Wing et al (2011), mainly represents that of Wing and Gould, who wrote in 2002, both together and separately they do not view PDA as a distinct syndrome. Wing and Gould argued that PDA features and behaviours are seen throughout the entire human population, although they note Newson’s work to be clinically useful (Christie, 2007; Milton, 2017; Wing, 2002). Interestingly, Wing et al (2011) suggest PDA might be a “double-hit”, that PDA features may not be caused by autism in autistic persons.
The initial reason why I place Wing et al (2011) below Eaton and Weaver (2020), is that the former note that persons can transition between autism subtypes, and argue this applies to all proposed subtypes, which includes PDA. What this means is that autistic persons can transition into PDA, and so PDA features do not need to present from birth. Wing consistently expressed such views of autistic persons transitioning between subtypes throughout her work from at least 1991 (Frith, 1991; Wing, 2002). As PDA does not need to be expressed since early infancy it is broader than the definitions of Eaton and Weaver (2020).
It must be said that Elizabeth Newson also noted that persons can transition into PDA, so it does not have to be from early infancy (Newson, 1989; 1999; Newson et al, 2003). However, Newson viewed PDA to not be a form of autism (Newson 1983; 1989;1996; Newson et al, 2003), and included non-autistic persons in her cohort (see below for more details). It is for this reason why I have ranked Wing et al (2011) diagnostic threshold to be above Newson et al (2003), as Wing and colleague’s threshold represents the boundary of autistic population and non-autistic persons in the diagram.
Richard Soppitt (2021) in a book chapter discusses Wing and Gould’s views on PDA, utilises a case study and a variation of the DISCO 11, PDA questions to highlight how PDA can be conceptualised. The chapter is useful in allowing us to further probe differences between Wing et al (2011), and Eaton and Weaver (2020) PDA thresholds. Soppitt argues PDA demand avoidance is pervasive in nature, in line with Eaton and Weaver (2020). There seems to be divergence in nature of the demand avoidance pathologized by Wing and Gould, versus and Eaton and Weaver. The latter demand avoidance is “often seemed illogical or perverse” (Eaton and Weaver, 2020, p37).
The case as described by Soppitt (2021), seems to be about pervasive non-compliance, often resulting from narrow and/ or rigid cognition in autistic persons. That an autistic CYP can be described with PDA, if they have narrow views, such as with games, do not conform to rules/ social expectations in most situations as the classroom setting or when lining up. Pertinently, the autistic CYP has a limited range of behaviours on how to cope when distressed, and can be easily triggered, such as when presented with doing a task not of their choosing. Soppitt mentions that case study will try every trick in the book to avoid requests of not their choosing, or even ask questions repeatedly for an hour to achieve what they wish.
This contrasts sharply to the demand avoidance outlined by Eaton and Weaver (2020), which can potentially include the CYP not eating when hungry. The demand avoidance as presented by Soppitt, is more because the autistic person does not agree with cultural and societal norms. Many persons would accept that autistic persons are often rational and logical, in fact this is meant to be a strength of autistic persons which should be highly valued by employers. One could argue that some of the pervasive non-compliance does results from autistic CYP not understanding non-autistic social norms. Which may be accurate in some cases and situations.
Newson et al (2003) specific trait is “Continues to resist and avoid ordinary demands of life” p597. Specifically relates to non-compliance of ordinary (non-autistic social and cultural norms). The non-compliance does not require a person to understand or not ordinary social norms, or even for the demand avoidance to be pervasive. Point I am making here is that Wing and Gould’s PDA definitions as described by Soppitt are not often inherently illogical or perverse as put forward by Eaton and Weaver (2020); i.e., the demand avoidance can be for rational or for reasonable reasons, such as triggers to known trauma (trains is given in the case study). Highlights how Wing and Gould’s PDA definitions are clinically broader than Help4Psychology’s.
I think that Wing and Gould’s clinical population, when added to their respective backgrounds, contributed to having different interpretations on PDA to Newson. Likewise, I think Newson’s own clinical background and clinical populations affected her own views on PDA. Such a comment can be applied to other PDA experts, one could see how Christopher’s background overlaps the clinical populations he predicts PDA to be in (see Gillberg, 2014). The reason why I am saying is this because I think Wing and Gould’s PDA population (all autistic), is different to Newson’s (included some non-autistic persons).
For example, Newson consistently viewed PDA’s social communication issues to be in deficits in social identity, pride and shame, and there are no Theory of Mind and Empathy deficits in PDA (Newson, 1989; 1996; 1999; Newson et al, 2003). That persons with PDA “button press” others to remove demands. Wing and Gould instead suggest that there are Theory of Mind issues in PDA and socially manipulative behaviour in PDA is random, becomes conditioned by attention received from others negative reinforces the act (Soppitt, 2021). Wing argues that all autistic persons, regardless of subtype can gain reward from upsetting others (2002). Wing and Gould’s comments on such behaviours are the product of reinforcement from other’s attention is plausible and are supported in Harry Thompson:
“Thompson would frequently respond to dares and act outrageously to gain attention, as others would react in a specific manner. Over time such behaviours were internalised and became part of his identity.” (Woods, 2019a, p95).
It remains to be seen how much of some PDA behaviours are habituated through various reinforcement processes. Newson required PDA to have Coding issues (when a person struggles to process or understand certain aspects of communication) to fit in her own 1986 constructed Pervasive Developmental Coding Disorders diagnostic grouping (Newson, 1989; 1996). The differences in their respective clinical populations should be considered when comparing their respective views on PDA.
Newson et al (2003) is a lower diagnostic threshold and discussed next.
Newson et al (2003).
We know that the Elizabeth Newson Centre, which diagnosed many persons with PDA, had inconsistent record keeping when diagnosing PDA in the mid-1990s (Graham-White, 2002). In their supplementary notes, Newson et al (2003) state:
“Clearly no child will show all the behavioural examples listed, any more than all autistic children show the whole repertoire of autistic behaviours; but every child with clear-cut PDA will manifest the overall complex pattern, not merely one or two features.”
Already mentioned, Newson required all persons with PDA to have socially manipulative demand avoidance (Newson et al, 2003). Other features while being common, were not universal among her sample, for example the Passive Early History trait was seen in 88% of her cases (only 12% were active in some way in the first year) (Newson et al, 2003). In some respects, there is some consistency to what features are being diagnosed in persons with PDA in Newson’s database. Newson stated that persons can transition into PDA (Newson, 1989; 1999; Newson et al, 2003). Furthermore, she saw some less clear-cut cases of PDA (Newson 1983; Newson, 1989), and removed cases that had features of autism from her cohort (Newson et al, 2003). While many cases of PDA, could receive a diagnosis of Pervasive Developmental Disorder – Not Otherwise Specified (PDD-NOS) or Atypical Autism (Christie 2007; Christie et al, 2012; Newson, 1983; Newson et al, 2003), this was not reported to be universal for Newson’s cases of PDA. Similarly, some argue that many of Newson’s cases would receive an autism DSM-5 diagnosis (Eaton and Weaver, 2020; Soppitt, 2021), this would not be applicable to the entire cohort. It is reasonable to assume that Newson’s PDA database contained some non-autistic persons.
Newson’s version of diagnostic grouping for Pervasive Developmental Disorders, included Specific Language Impairments and PDA, which are not forms of autism, and her definition for PDD-NOS is when a person does not meet the threshold for either Autistic Disorder, Asperger’s Syndrome, PDA and Specific Language Impairment (Newson, 1999; Newson et al, 2003). This definition is broader than the accepted version which is used for when a person did not meet the threshold for Autistic Disorder of Asperger’s Syndrome (American Psychiatric Association, 1994). Newson also viewed the autism spectrum to only be comprised of Autistic Disorder and Asperger’s Syndrome (see supporting notes to Newson et al, 2003). While the accepted version of DSM-4 autism spectrum includes Autistic Disorder, Asperger’s Syndrome and PPD-NOS (Christie et al, 2012; Green et al, 2018). That a person with her version of PDD-NOS could transition into any of these four syndromes, i.e., non-autistic persons can transition into PDA. Later, Christie (2007), stated that PDA would be used to reclassify large numbers of persons who received a PDD-NOS (APA PDD-NOS definition) diagnosis with PDA. That a substantial amount of the autistic population was meant to receive a PDA diagnosis under the views of Christie (2007).
These aspects combine to tell us that Newson had a lower diagnostic threshold for PDA, than Eaton and Weaver (2020), as a person did not need to have PDA from early infancy, and her database included non-autistic persons. That under Newson et al (2003) approach to PDA, that it is a relatively common mental disorder.
It must also be stressed that the developmental traits of neurological involvement, passive early history and speech delay were made optional for PDA diagnosis in 2015 (O’Nions et al, 2016a). Since then, it has been common to portray PDA diagnostic traits without the developmental aspects (Fidler, 2019; Fidler and Christie, 2019; Green et al, 2018; Russell, 2018). The most common PDA diagnostic tool has no questions to assess for developmental features (O’Nions et al, 2016a). Which adds to the point that Eaton and Weaver (2020) is a high diagnostic threshold for PDA.
Comments on Wing and Gould’s premature critique of Newson’s research.
Wing critiqued Newson’s PDA research independently of Gould (Wing, 2002), and co-authored with Gould in 2002 (Christie, 2007; Milton, 2017), this was a year before Newson et al (2003) work was published. It matters as the original PDA DISCO questions are based on Newson’s unpublished research (Gillberg et al, 2015; O’Nions et al, 2014; O’Nions et al, 2016). For example, Newson et al (2003) wrote there is not sufficient evidence yet for Neurological Involvement trait as it has not been sufficiently researched. Despite this Wing and Gould created two questions to assess for Neurological Involvement: “Clumsy in gross movements” and “Hands seem limp and weak for unwelcome tasks” (Gillberg et al, 2015, p980). Gillberg et al (2015) with their low PDA diagnostic threshold, only requires either question 13 or 14 to be present and five other questions to be a yes, for a “Classic PDA” diagnosis; found in their sample that clumsiness is among the most common features for “Classic PDA”, in 89% of their PDA cases. Newson et al (2003) mention that CYP with PDA motor movement tends to be clumsy, in their supplementary notes about 75% of their Study B CYP with PDA were clumsy. It seems that Gillberg et al (2015) found being clumsy is more common in PDA than Newson et al (2003).
Later Soppitt provides a case study using a variation of the original PDA DISCO questions and while discussing how their case study:
“His hands seem limp for unwelcome task (Y). He uses every trick in the book to avoid complying to avoid with requests not to his choosing” (Soppitt, 2021, p301).
This is rather a generic and an all-encompassing statement which seems to be about demand avoidant behaviours, not features associated to neurological features. Effectively, the case study has had more of their actions pathologised as demand avoidance using a question designed for a trait, which might not be a stable or part of PDA. This suggests there is some confusion over the purpose of this question and the nature of Newson’s observations. Vitally, it also suggests that at least three different clinics are seeing different versions of PDA. With Newson seeing limp hands as sign of neurological involvement. Gillberg et al (2015) potentially seeing clumsy motor coordination more often than Newson did and the case study by Soppitt attributing the feature of limp hands as part of manipulative social demand avoidance trait. Supporting the outlook there is no consensus over how to view PDA, or how to assess for it (Langton and Frederickson, 2016; O’Nions et al, 2014a; O’Nions et al, 2016). It is plausible that Wing and Gould’s premature critique of Newson’s work and early creation of the original PDA DISCO questions has contributed to the diversity of PDA outlooks.
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) Obsessive-Compulsive Disorder (OCD).
I think there is a substantial gap between this threshold, and Newson et al (2003) and Eaton and Weaver (2020). For many reasons, which I do not have space to go into here, I am currently viewing PDA as an OCD and Related Disorder, so not part of the autism spectrum. Key reasons are discussed below.
PDA’s central impairment is high anxiety driven demand avoidance, and anxiety is recognised to be a co-occurring difficulty to autism (Egan et al, 2019; Gould and Ashton-Smith, 2011; Woods 2020a). Newson et al (2003) conceptualised the demand avoidance as being obsessive in nature, and Christopher Gillberg questions if it is a new type of mental disorder (2014). In OCD, there is a simplified cycle of thoughts and actions (OCD-UK, 2020), that matches what happens in PDA. The OCD cycle starts with an obsession (demand), which then causes anxiety or distress to an individual. The individual then responds to the obsession with a compulsion, which is an act or thought that attempts to resist, ignore, remove the obsessive thought. Subsequently, the individual experiences temporary relief from their anxiety and distress, even only for a few moments until the next obsessive thought.
There is a hierarchy of behaviours that persons tend to display when asserting their self-agency with others. For example, a person will tend to initially express: distraction, then making excuses, before moving onto physical self-incapacitation, or using fantasy and roleplay and finally displaying extreme behaviour like violence or running away. The options and different levels of behaviours a person may express when asserting their self-agency are shown below, in the PDA Society (2021) image.
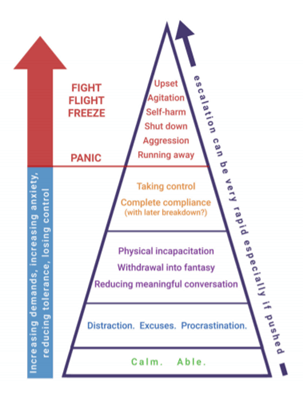
I am not entirely happy with this diagram, as I think a person is likely to be highly aroused at the lower levels. Also, just because a person is calm, does not intrinsically mean they are “able”. If a person is highly aroused, they are unlikely to be thinking logically, or rationally. So, the more anxious and distressed a person is, the less information they will tend to be processing, which is why I dislike the dichotomy between panic response and non-panic response; it suggests that a person can be rational and relatively in control of their actions before panicking. This contradicts understandings of how a person’s cognitive processes work when highly aroused.
The reason why I am showing this diagram is to show that withdrawing into fantasy and roleplay is a copying mechanism in PDA (Newson, 1983), it is intrinsically an RRBI, that is expressed as part of the demand management cycle. Meaning that the associated PDA trait is represented as part of the OCD DSM-5 threshold. Socially manipulative demand avoidance, avoidance of ordinary demands and obsessive behaviour are also represented at this PDA diagnostic threshold. The lability of mood, not so much, considering this trait is not universal in Newson’s cohort (Newson et al, 2003), and how a PDA diagnosis is about assisting persons; it seems to short sighted and unethical to deny a person a PDA diagnosis at this threshold just because lability of mood features may not be present.
A fundamental reason for this is that anxiety based RRBIs while seen in some autistic persons are features associated with the Triad of Impairment of autism (even recently Dyad of Impairment). Other pertinent reasons include that much, or most PDA behaviours are obsessive in nature (Newson et al, 2003), and the demand avoidance has been described as compulsive in nature (Ayres, 2015). Secondly, research from PDA caregivers suggests that PDA follows the OCD cycle (O’Nions, 2019), to produce the Demand Management Cycle, as shown below:

An example of the Demand Management Cycle describing demand avoidance in PDA. A young autistic child has the demand to attend school. The child becomes anxious from the prospect of facing sensory overload during class and bullying at break times. The child avoids the demand to attend school through school refusal and in the process gains relief from the anxiety of facing a known distressing situation, until the next time they are faced with that demand. It can be more complicated than this in real life, with the caregivers attempting multiple times for the child to attend school each day for multiple weeks, and in response the child escalates their behaviours to the aversive demand. The child might start with attempting to negotiate with the adult, as this attempt fails, might try to incapacitate themselves. Finally, the child becomes violent to the caregiver, and at this point the demand to attend school is withdrawn for that day. This scenario conforms to understandings of OCD, as the distressing thoughts, are inherently the child’s perspective. The compulsive school refusal and violence towards the caregiver would cause clinically significant distress and impairment in social and an area of functioning, educational (OCD-UK, 2020).
The above example is in line with the “Rational Demand Avoidance” group reported by Eaton and Weaver (2020), in which autistic CYP presented PDA behaviours, often after experiencing aversive situations at school (Eaton, 2018). This group seems to be for those not meeting Eaton and Weaver (2020) threshold for a PDA diagnosis, as their behaviours are not pervasive in nature. I would point out that if an autistic person is expressing PDA behaviours over an extended period, it is in the best interests of the child to receive a PDA diagnosis, to prevent them experiencing more trauma, that we know can be with them for the rest of their lives (Rumball et al, 2021). This approach is in-line with the multi-agency PDA assessment pathway, which is partly there to prevent deterioration in the presentation of autistic CYP (Summerhill and Collett, 2018). At this diagnostic threshold, demand avoidance is not necessarily from demands like brushing their teeth, or drinking water, it is a lower threshold than Newson et al (2003).
Extreme Demand Avoidance-Questionnaire (EDA-Q) Threshold.
I will be honest, I am unsure if the EDA-Q threshold is lower or higher than the DSM-5, OCD diagnostic threshold. I think they are around a similar level. I will explain why.
The EDA-Q is a 26-item observer rated questionnaire for 5 – 17 years old, up to mild intellectual difficulties (O’Nions et al, 2014). The questions are scored from 0 – 3, on four anchor points. It has two cut-offs, one of 50+ for 5 – 11-year-olds and 45+ for 12 – 17-year-olds. The EDA-Q only has one question that assesses developmental traits, which is “S/he was passive and difficult to engage as an infant” (O’Nions et al, 2014, p763). The EDA-Q is designed to assess for demand avoidance of manipulative behaviours. All the core 5 traits are represented among its questions (O’Nions et al, 2014), and this is how it is higher than the Gillberg et al (2015) diagnostic threshold.
As part of developing the EDA-Q, 10 clinicians were consulted, and most of them self-reported seeing less than 20 cases of PDA throughout their professional careers. Likewise, many are from highly specialised autism settings (O’Nions et al, 2014). This raises two questions? Are their views representative of how PDA presents in the general population? Are these clinicians seeing the same construct, at the similar diagnostic thresholds and prevalence rates?
The actual article views PDA as being part of the autism spectrum, “Their apparently intact awareness of how to ‘push people’s buttons’ suggests a level of social insight that is unusual in children with ASD.” (O’Nions et al, 2014). The participants were allocated to 6 different groups; however, the PDA groups were directly filtered against two groups containing autistic CYP, see Figure 1 in O’Nions et al (2014, p761). The CYP with PDA reported, were split into two groups, 50 confirmed PDA diagnosis, and 67 suspected cases of PDA. The participants were not screened for autism, instead it relied upon reported caregiver diagnoses and who were potentially autistic. The CYP in this research were only screened with 32 candidate EDA-Q items and the Strengths and Difficulties Questionnaire (O’Nions et al, 2014).
This is important as the article (and many others) note there is no consensus over how to view PDA, or how to formally diagnose PDA (O’Nions et al, 2014). There is no feature specific to PDA (Eaton and Weaver, 2020; Woods, 2019b; Woods 2019c), and PDA behaviour profile overlaps many other conditions, with many predicted populations (Gillberg, 2014; Green et al, 2018; Woods, 2019b). The other diagnoses of the two PDA groups are not reported, especially if they have an autism diagnosis or not. When at the time of the research being conducted in 2010 – 2012/ 2013, PDA was mainly diagnosed independently of autism, for other examples see (Carlile, 2011; Harvey, 2012; Jones, 2005; Langton and Frederickson. 2016a; Langton and Frederickson, 2016b; Newson et al, 2003). As established in a prior section, autism is more narrowly defined than PDA, due to the latter being a Pervasive Developmental Disorder. These factors combine to mean we cannot be sure, how many of the CYP with PDA in O’Nions et al (2014) sample are autistic, it is likely to contain many non-autistic CYP.
O’Nions et al (2014) refer to unpublished research of O’Nions et al (2015) that persons with PDA have autistic-like features comparable to autistic persons. Digging deeper into this claim there are a few problems. First, it is possible to meet clinical threshold for autism and not be autistic, as per “quasi-autism” cases of Attachment Disorder (Flackhill et al, 2017). Furthermore, it is possible for autistic persons to be misdiagnosed with other conditions, for instance this notoriously frequently happens with Borderline Personality Disorder (Eaton, 2017; Milton, 2017). The sample size for O’Nions et al (2015) is relatively small at 14 persons. Additionally, caregivers were sourced from persons known to the research team and had high amounts of PDA relevant behaviours. O’Nions et al (2015) note several CYP had traumatic experiences and there were not unusually difficult or abusive backgrounds. Richard Soppitt (2021) discusses how most cases of PDA have some aspects of trauma, and how he views PDA as mainly represented by ADHD and trauma. One CYP is known to be diagnosed with Attachment Disorder and scored exceptionally low on an autism diagnostic tool.
It must be stated that O’Nions and others have been approaching PDA from their understanding of autism (O’Nions et al, 2016b). This is opposite of how scientific-method research is conducted, as one should not be prioritising their beliefs over other perspectives (Woods, 2019b). It is difficult to take much from O’Nions et al (2015) besides that O’Nions et al (2015) preconceived notions of PDA are autism-like, but it is insufficient evidence to equate PDA to autism, or to assume that all CYP with PDA in O’Nions et al (2014) are autistic.
This matters when PDA is not defined as being part of the autism spectrum. The EDA-Q was designed to discriminate PDA in autistic CYP. Effectively, in O’Nions et al (2014) we do not know if the EDA-Q threshold is discriminating autistic persons with PDA, or non-autistic persons with PDA, from autistic persons without PDA. Those who view PDA as a form of autism, often dislike the EDA-Q as it supposedly has a high rate of false-positives, i.e., identifying non-autistic persons with PDA when it is not meant to be. I would counter and say, O’Nions et al (2014) validated the EDA-Q to also detect PDA in non-autistic CYP, as well as in autistic CYP with PDA. This explains why some research detects PDA in non-autistic persons (Eaton, 2018; Flackhill et al, 2017; Green et al, 2018; Reilly et al, 2014). This tells us that the EDA-Q detects PDA much more often than the Eaton and Weaver (2020) diagnostic thresholds.
I have discussed the various diagnostic thresholds and how they relate to each other, and in the process why they are placed where they are on the diagram. I need to detail my preferred PDA diagnostic threshold, and this is done below.
Directly comparing Gillberg et al (2015) and EDA-Q Threshold.
Original PDA Questions.
2: Comfortable in role play and pretending. – 3, 7.
2: Continues to resist and avoid ordinary demands of life. Strategies of avoidance are essentially socially manipulative. – 13, 14.
2: Lability of mood, impulsive, led by need to control. – 5, 6,
0: Language delay, seems result of passivity. – 0
2: Neurological involvement. – 2, 8.
5: Obsessive behaviour. – 7, 9, 10, 12, 15.
1: Passive early history in first year. – 1,
6: Surface sociability, but apparent lack of sense of social identity, pride, or shame. – 4, 6, 11, 12, 14, 15.
EDA Questions.
5: Comfortable in role play and pretending. – and distractedness (1 item), mimicry and role play (4 items).
7: Continues to resist and avoid ordinary demands of life. Strategies of avoidance are essentially socially manipulative – perceived pressure (1 items), purposes of avoidance or controlling interactions (6 items),
5: Lability of mood, impulsive, led by need to control – need for control (2 items); emotional lability in response to demands (3 items).
Language delay, seems result of passivity. –
1: Neurological involvement. – 30 floppiness during infancy (1 item)
0: Obsessive behaviour. –
1: Passive early history in first year. – 29 passivity (1 item).
9: Surface sociability, but apparent lack of sense of social identity, pride, or shame. – lack of responsibility (3 items), insensitivity to hierarchy/ praise/need to manage reputation (6 items).
2: Do not fit with any trait. communicative difficulties (2 items)
I suspect that obsessive features of PDA are represented in the questions, but it is not directly attributable to the trait as O’Nions et al, did not design the EDA-Q for its questions to directly match its traits. For example, question One “Obsessively resists and avoids ordinary demands” p763, is in line with Newson described PDA demand avoidance to be obsessive in nature. It is possible that some others might attribute different questions to different traits. I have tried to follow the designated groups used by O’Nions et al and to match them to the clinical descriptions of Newson that underpins the development of the EDA-Q.
Table 2: PDA diagnostic traits and the number of corresponding questions in the EDA-Q and 15 Original PDA DISCO questions.
| PDA Trait. | Number of EDA-Q Questions that assess it. | Number of EDA-Q Questions that assess it. |
| Comfortable in role play and pretending. | 5 | 2 |
| Continues to resist and avoid ordinary demands of life. Strategies of avoidance are essentially socially manipulative. | 7 | 2 |
| Lability of mood, impulsive, led by need to control. | 5 | 2 |
| Language delay, seems result of passivity. | 0 | 0 |
| Neurological involvement. | 1 | 2 |
| Obsessive behaviour. | 0 | 5 |
| Passive early history in first year. | 1 | 1 |
| Surface sociability, but apparent lack of sense of social identity, pride, or shame. | 9 | 6 |
| Total. | 28 | 20 |
There were 30 items that only assess one trait once in the EDA-Q. Two items assessed social communication issues relating to autism and not PDA traits; so, the EDA-Q total is 28. For original 15 PDA DISCO questions, 10 questions only assess, 1 trait, while 5 questions simultaneously assess 2 PDA traits; so that they their total is 20.
Developmental traits are underrepresented in both tools, although better represented in the original 15 PDA DISCO questions, for instance 2 questions assessing for Neurological Involvement, compared to 1 item in the EDA-Q. Neither tool directly assesses for speech delay. Although, the full DISCO contains questions that assess for speech delay, and the question booklet in the O’Nions et al (2014) contained two questions that asked when the child began to speak words and phrases.
Some criminal behaviour, like harassment in the DISCO questions are viewed as obsessive behaviour (Gillberg et al, 2015). The EDA-Q questions are partly derived from the original PDA DISCO questions (O’Nions et al, 2014). One might assume that while the EDA-Q questions are not described as assessing for Obsessive Behaviour trait, some questions actually do, e.g., “Knows what to do or say to upset specific people” (O’Nions et al, 2014, p763), seems to be derived from “Lies, cheats, steals, fantasises, causing distress to others” (Gillberg et al, 2015, p980). Crucially, the latter question is partly attributed to Obsessive Behaviour trait, indicating the EDA-Q question is assessing for a CYP knowing how to cause distress to someone they are obsessed with.
The EDA-Q was designed to view PDA behaviours as being manipulative in nature, i.e., the person has intent to misled and/ or control other persons. This observation unnerves me as it undermines O’Nions more recent view that PDA social demand avoidance should be viewed as strategic, as CYP with PDA behaviours are not as sophisticated as persons who have callous-unemotional traits (O’Nions and Eaton, 2020). If the behaviours are being displayed for the same reasons, to control others for one’s own aims then said behaviours would still be manipulative, irrespective if they are less “sophisticated”. PDA is not believed to have Theory of Mind deficits (Christie et al, 2012; Newson et al, 2003). This is a tangent, the purpose of the table is to show that it is easier to meet diagnostic threshold for PDA under Gillberg et al (2015), than threshold under EDA-Q.
Gillberg et al (2015) diagnostic threshold is:
“Classic PDA” was defined as Total PDA score of 5 or more and including the presence of socially manipulative or shocking behaviour to avoid demands.” (Gillberg et al, 2015, p981).
The mandatory features are represented by question 13 “Socially manipulative behaviour to avoid demands” (ibid, p980), and question 14 “Socially shocking behaviour with deliberate Intent” (ibid, p980). The other 13 questions assess for 6 other PDA traits, it is possible for someone to meet Gillberg’s “Classic PDA” threshold without many of the other core PDA traits present. For instance, the common trait seen in Gillberg et al (2015) persons with PDA, was Neurological Involvement (along with Lability of Mood and Comfortable in Roleplay and Pretend), which Newson stated it remains to be seen if there is sufficient evidence to include (Newson et al, 2003). This is a tangent.
The EDA-Q overwhelmingly assesses for core PDA traits and surface sociability trait, which means for a person to meet the EDA-Q’s lowest threshold of 45, a person is likely to have features representing the core traits. EDA-Q has 26 questions with, scored on 4 anchor points, from 0 – 3. Even if one scores 27 on all 9 surface sociability, it still means a person needs to answer 6 other questions to achieve cut-off, which are likely to be representative of other traits. The EDA-Q has a more even distribution of questions per trait, for the core traits and surface sociability, ranging between 5 – 9. While the original 15 PDA DISCO questions have a huge range of 2 – 5 questions per trait, for the core PDA traits. A person diagnosed using the EDA-Q, compared to the “Classic PDA” with original PDA DISCO questions, is more likely to have features representing the core PDA traits present.
MY PREFERRED PDA DIAGNOSTIC THRESHOLD.
I think that the Gillberg et al (2015) threshold is too low, as it does not require the 5-core anxiety based RRBIS to be present. However, my view is that the PDA diagnostic threshold should be around the DSM-5 OCD threshold and/ or the EDA-Q threshold. That the 5 core traits be present in some capacity and that the demand avoidance follows the Demand Management Cycle. There are few reasons for this. Firstly, there is no consensus over what PDA is, or how it presents, and how to diagnose it (Christie 2007; Flackhill, 2017; Gillberg 2014; Green et al, 2018; Milton, 2017; O’Nions et al, 2014; O’Nions et al, 2016a; Woods, 2020b).
Accounting for this, it is ethical to take a broad and inclusive approach to conceptualising PDA, as otherwise would be to remove the PDA diagnoses of many persons diagnosed at lower thresholds. Such an approach directly contradicts a central argument of PDA is that it is required for specific strategies, and to better explain a person’s actions to all stakeholders (Christie, 2007; Christie et al, 2012; Newson, 1989; Newson et al, 2003; O’Nions et al, 2016a). Furthermore, it would contradict a consistent reason for Newson reifying PDA’s behaviour profile and creating her own diagnostic grouping (see Newson, 1989; 1996), that such entities should benefit lay persons, including caregivers (Newson, 1989; 1996; Newson et al, 2003). Adopting the lower threshold would also mirror inclusive practice adopted the Neurodevelopmental Disorders Workgroup to allow those with a “well-established” DSM-4 autism diagnosis (Asperger’s Syndrome, Autistic Disorder and Pervasive Developmental Disorder – Not Otherwise Specified) to viewed as having an DSM-5 ASD diagnosis; said individuals would still receive appropriate support (Rosen et al, 2021).
As mentioned earlier, a PDA diagnosis is vital to helping to prevent presentations of autistic CYP deteriorating due to a lack of appropriate support (Summerhill and Collett, 2018) and being more adversely impacted by trauma (Rumball et al, 2021). This reflects the arguments for diagnosing PDA, that rely upon universal rights (Summerhill and Collett, 2018). Even though the EDA-Q is not designed to diagnose PDA (O’Nions et al, 2016a), and it has several limitations (Woods, 2020a); the tool has been used to assist diagnosing PDA (Lyle and Leatherland, 2018; Reilly et al, 2014; Summerhill and Collett, 2018).
The EDA-Q was used to produce the most used PDA diagnostic questions (O’Nions et al, 2016a). Most of the PDA research has been conducted using the EDA-Q (Bishop, 2018; Brede et al 2017; Doyle et al, 2020; Eaton, 2018; Egan et al, 2019; Goodman, 2018; Green et al, 2018; Langton and Frederickson, 2016a; Langton and Frederickson, 2016b; Lyle & Leatherland, 2018; Moore, 2020; O’Nions et al, 2014, 2015; O’Nions et al, 2018a; Reilly et al, 2014; Stuart et al, 2020; Woods, 2019c). Adopting a higher diagnostic threshold essentially discards this research, as we cannot be sure that it is directly appropriate to generalise these results onto those of a narrower, stricter definitions. The opposite of this is that we cannot be sure that we can generalise results onto lower and broader PDA diagnostic thresholds.
Adopting these threshold’s also fit into our modern understandings of how PDA is transactional, and it respects divergent opinions that PDA is seen outside of autism (Christie 2007; Gillberg, 2014; Green et al, 2018; Woods, 2020b). Pertinently, it respects research results suggesting PDA is seen in non-autistic persons (Woods, 2019b; Woods, 2020b). Moreover, adopting these thresholds allows us to investigate predicted PDA populations, with an established threshold, that maintains the fundamental aspects of PDA. Thus, meeting ethical requirements to be attempted to falsify one’s perspectives and not biasing one perspective over another (Woods, 2019b). Furthermore, how highly contested PDA is and lacking consensus over what PDA is and how to diagnose it, undermines the case for any clinician, or group of clinicians to reasonable argue that a high PDA diagnostic threshold is a suitable conceptualisation of PDA.
I propose that persons utilising this diagnostic threshold’s use specifiers to indicate the areas that demand avoidance is impairing a person, such as:
- Educational.
- Occupational.
- Pervasive (all).
- Social.
That the 5 core traits be present in some capacity and that the demand avoidance follows the Demand Management Cycle.
These are all the reasons I have for adopting this diagnostic threshold, I recall at the time of writing. There are probably other reasons to adopt this outlook, I encourage others to consider what I put forward here and to discuss its merits and weaknesses.
IMPLICATIONS OF THIS DIAGRAM.
I discuss some implications of what proposed above, but I am raising some further implications here. More pivotal questions to consider going forward and practices that PDA stakeholders should adopt.
Something that is overlooked, is that Christopher Gillberg proposes to rename PDA with “Extreme Demand Avoidance” (2014), he discusses how he thinks PDA is a common mental disorder and possibly a new type of mental disorder. Gillberg’s conceptualisation of PDA is arguably the broadest and most inclusive perspective on PDA, encompassing “Extreme Demand Avoidance” as described by Eaton and Weaver, and their “Rational Demand Avoidance” groups, demonstrating the arbitrary nature of this division. Crucially, when added to how Wing and Gould view PDA to be pervasive non-compliance, which can often be for rational and logical reasons by autistic persons. PDA being about non-compliance seems to be supported by Phil Christie who describes school refusal (anxiety impacting willingness to attend school) as “the ultimate avoidance” (Christie, 2007, p8) It is reasonable to call ALL conceptualisations of PDA “Rational Demand Avoidance”, as proposed by autistic persons like myself and Damian Milton (2017).
Is research using higher diagnostic thresholds, representing the same construct? Is adopting strict definition discarding most PDA research, which is conducted at lower thresholds?
There is clearly no single definition of PDA. This means there is no single understanding of PDA to maintain integrity over.
Eaton and Weaver (2020) claimed they examined the current literature. Their PDA definitions seem to be at the extreme end of PDA diagnostic threshold’s. Pertinently, are not representative of broader PDA threshold’s: like used by Wing et al (2011); or those using the EDA-Q (Lyle and Leatherland, 2018; Reilly et al, 2014; Summerhill and Collett, 2018); or the “Classic PDA” of Gillberg et al (2015) which is substantially lower diagnostic threshold than Eaton and Weaver (2020).That other PDA experts removed developmental traits from PDA diagnostic criteria (Fidler, 2019; Fidler and Christie, 2019; Green et al, 2018a; Russell, 2018). That Newson did not require a person to show PDA features or traits to receive a PDA diagnosis (Newson et al, 2003).
O’Nions and colleagues (2018b) argued that there is a need for more research into interventions for “problematic demand avoidance” in autism, and presumably PDA would be diagnosed for a person to receive such interventions. However, what is problematic demand avoidance is highly subjective and more encompassing than just “pervasive” demand avoidance. If a CYP is school refusing or meeting cut-off on the EDA-Q, they are likely to be highly distressed and causing substantial problems for those around them. Particularly, concerning is that if a 5 – 7-year-old autistic CYP is displaying PDA behaviours after experiencing aversive experiences such as school (Eaton, 2018). Then said autistic CYP is likely to struggling to manage and process the behaviours they are expressing, such as frequent “tantrums”/ kicking/ hitting (O’Nions et al, 2014). Help4Psychology’s “Rational Demand Avoidance” group would fit into “problematic demand avoidance”, that there is a need for urgent intervention research, and presumably diagnosing these CYP with PDA.
Historically, the demand avoidance was centred on non-compliance to social and cultural norms. Christie views school refusal as “the ultimate avoidance” (2007, p8). That research was required to investigate why non-autistic CYP comply with demands, while CYP PDA do not (Christie et al, 2012; Happé and O’Nions, 2011). This means that at least traditionally, PDA demand avoidance was not concerned about it being irrational/ perverse in nature; contradicting Eaton and Weaver (2020) PDA definitions (Although, one could view this change as an example of looping effects in action, see Woods, 2017 for more details). Summerhill and Collett (2018) detail a multi-agency assessment pathway for PDA (partly originally designed by Judy Eaton), whose purpose includes preventing deteriorating presentations in autistic CYP.
Eaton and Weaver did not need to use their informal algorithm, information relating to some other diagnostic thresholds are publicly available in the literature, these include: EDA-Q threshold (O’Nions et al, 2014a); Gillberg et al (2015); Newson et al (2003), while Newson’s diagnostic tools is not publicly available, a 22 question semi-structured interview derived from original PDA DISCO questions and Newson’s research is (O’Nions et al, 2015; O’Nions et al, 2018a). It was possible for Eaton and Weaver to replicate these diagnostic thresholds. Moreover, at least one clinician at Help4Psychology has diagnosed PDA as a standalone diagnostic entity in Eaton and Banting (2012), although they did view PDA to be part of the autism spectrum. This Raises questions:
- What exact features Help4Psychology observed when they reviewed the literature to adapt these strict definitions (I am aware that not all the information in this blog would have been available to Eaton and Weaver at time of them constructing their definitions)?
- Even, if only examining the literature in 2015, before started data collecting; what particular features justified their definitions?
- How are Help4Psychology PDA thresholds representative of broader clinical practice on PDA?
Help4Psychology research is not a large scale trails needed to establish nosology and validity and is essentially a clinical audit.
When talking about PDA, researchers and clinicians need to specific:
- What certain definition for PDA they use.
- What exact behaviour profile they are using, particularly the wording as different versions have different clinical interpretations.
- What their exact threshold for PDA is.

REFERENCES.
American Psychiatric Association. (1994). Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC, American Psychiatric Association.
Ayres, N. (2015). Can’t Help Won’t – Pathological Demand Avoidance Syndrome (Newspaper article). Retrieved from: https://www.huffingtonpost.co.uk/neil-ayres/cant-help-wont-_b_7783632.html?guccounter=1&guce_referrer=aHR0cHM6Ly93d3cuZ29vZ2xlLmNvLnVrLw&guce_referrer_sig=AQAAALd1cbe8MNnBt6eh_dAquPDhSJ9JyeQbb-6z_5_BoEvT-ErAfVsP1yN3hedTp7Vwduh_aiCW4FV5pl5jD4sfSIHyyHK4wB_Isfrb48Q7WbszVZYdSg0b2mGnZeUdbrM8K_tkykRSCT_ogMMwUxzfwK3WDXmMggUFRKkEzYmWQAW3 (Accessed 16 January 2021).
Bishop, E. (2018). The Relationship between Theory of Mind and Traits Associated with Autism Spectrum Condition and Pathological Demand Avoidance Presentations. Doctorate of Clinical Psychology, University College London.
Brede, J., Remington, A., Kenny, L., & Warren, K. (2017). Excluded from school: Autistic students’ experiences of school exclusion and subsequent re-integration into school. Autism & Developmental Language Impairments, 2(1), 1-20.
Carlile, J. (2011). Helping your child with PDA to play: eight strategies for supporting a child with Pathological Demand Avoidance Syndrome at home. Good Autism Practice, 12(2), 51-55.
Christie, P. (2007). The distinctive clinical and educational needs of children with pathological demand avoidance syndrome: guidelines for good practice. Good Autism Practice, 8(1), 3–11.
Christie, P., Duncan, M., Fidler, R., & Healey, Z. (2012). Understanding pathological demand avoidance syndrome in children: A guide for parents, teachers and other professionals. London: Jessica Kingsley Publishers.
Doyle, A., Kenny, N., & McNally, S. (2020). Mapping Experiences of Pathological Demand Avoidance in Ireland (Online Report). Retrieved from: https://www.pdasociety.org.uk/wp-content/uploads/2020/02/Doyle-and-Kenny-2020-Mapping-PDA-in-Ireland-Executive-Summary-1.pdf (Accessed 16 January 2021).
Eaton, J. (2017). A guide to mental health issues in girls and young women on the autism spectrum: diagnosis, intervention and family support. London: Jessica Kingsley Publishers.
Eaton, J. (2018). PDA and differential diagnosis (Conference paper). Retrieved from: https://www.autism.org.uk/what-we-do/professional-development/past-conferences/pda-2018-presentations (Accessed 16 January 2021).
Eaton, J., & Banting, R. (2012). Adult diagnosis of pathological demand avoidance – subsequent care planning. Journal of Learning Disabilities and Offending Behaviour, 3(3), 150-157.
Eaton, J., & Weaver, K. (2020). An exploration of the Pathological (or Extreme) Demand Avoidant profile in children referred for an autism diagnostic assessment using data from ADOS-2 assessments and their developmental histories. Good Autism Practice, 21(2), 33-51.
Egan, V., Linenburg, O., & O’Nions, L. (2019). The Measurement of Adult Pathological Demand Avoidance Traits. Journal of Autism and Developmental Disorders, 49(2), 481-494.
Fidler, R and Christie, P. (2019). Collaborative Approaches to Learning for Pupils with PDA: Strategies for Education Professionals. London: Jessica Kingsley Publishers.
Flackhill, C., James, S., Soppitt, R., & Milton, K. (2017). The Coventry Grid Interview (CGI): exploring autism and attachment difficulties. Good Autism Practice, 18(1), 62-80.
Frith, U. (1991). Autism and Asperger’s Syndrome. Cambridge: Cambridge University Press.
Gillberg, C. (2014). Commentary: PDA – public display of affection or pathological demand avoidance? – reflections on O’Nions et al. (2014). Journal of Child Psychology and Psychiatry, 55: 769–770.
Gillberg, C., Gillberg C., Thompson, Lucy., Biskupsto, R., & Billstedt, E. (2015). Extreme (“pathological”) demand avoidance in autism: a general population study in the Faroe Islands. European Child & Adolescent Psychiatry, 24(8), 979–984.
Goodman, A. (2018). Emotion Regulation and Executive Function in Children and Adolescents with Autism Spectrum Disorder and Pathological Demand Avoidance Traits. Doctorate of Clinical Psychology, University College London.
Gould, J., & Ashton-Smith, J. (2011). Missed diagnosis or misdiagnosis? Girls and women on the autism spectrum. Good Autism Practice, 12(1), 34–41.
Graham-White, C. (2002). An Investigation into the Communication Development and General Communication of children with Pathological Demand Avoidance Syndrome (Unpublished research). Retrieved from: https://www.autismeastmidlands.org.uk/wp-content/uploads/2016/10/Communication-development-of-Children-with-pathological-Demand-Avoidance-Syndrome.pdf (Accessed 16 January 2021).
Green, J., Absoud, M., Grahame, V., Malik, O., Simonoff, E., Le Couteur, A., & Baird, G. (2018). Pathological Demand Avoidance: symptoms but not a syndrome. Lancet Child & Adolescent Health, 2(6), 455–464.
Happé, F., & O’Nions, E. (2011). New research ideas and questions about PDA. In: National Autistic Society (Ed), Pathological Demand Avoidance Conference. Manchester: National Autistic Society.
Harvey, T. (2012). The educational issues for the child with a diagnosis of Pathological Demand Avoidance. Good Autism Practice, 13(1), 9-12.
Jones, E. (2005). Developing independence through the use of a colour-coded system with a fifteen-year-old pupil with a diagnosis of Pathological Demand Avoidance Syndrome (PDA) in a mainstream school. Good Autism Practice, 6.
Langton, E., & Frederickson, N. (2016a). Mapping the educational experiences of children with pathological demand avoidance. Journal of Research in Special Educational Need, 16(4), 254–263.
Langton, E., & Frederickson, N. (2016b). Parents’ experiences of professionals’ involvement for children with extreme demand avoidance. International Journal of Developmental Disabilities, 64(1), 16-24.
Lyle, C., & Leatherland, H. (2018). Preventing school exclusion: a case study of a primary aged autistic child with ADHD and a PDA profile. Good Autism Practice, 19(2), 33-42.
Milton, D. (2017). A Mismatch of Salience: Explorations of the nature of autism from theory to practice. Hove, UK: Pavilion Publishing and Media Limited.
Moore, A. (2020). Pathological demand avoidance: What and who are being pathologized and in whose interests? Global Studies of Childhood, 10(1), 39-52.
Newson, E. (1983). Pathological Demand-Avoidance Syndrome. Communication, 17, 3-8.
Newson, E. (1989). Pathological Demand Avoidance Syndrome: diagnostic criteria and relationship to autism and other developmental coding disorders (Research report). Retrieved from: https://www.autismeastmidlands.org.uk/wp-content/uploads/2016/10/Pathological-Demand-Avoidance-Syndrome.pdf (Accessed 16 January 2021).
Newson, E. (1996), Pathological Demand Avoidance Syndrome: a statistical update (Conference paper). Retrieved from: https://www.autismeastmidlands.org.uk/wp-content/uploads/2016/10/Pathological-Demand-Avoidance-a-statistical-update.pdf (Accessed 16 January 2021).
Newson, E. (1999). The Family of Pervasive Developmental Disorders (Online document). Retrieved from: https://www.autismeastmidlands.org.uk/wp-content/uploads/2016/10/The-family-of-pervasive-development-disorders.pdf (Accessed 16 January 2021).
Newson, E., Le Maréchal, K., & David, C. (2003). Pathological demand avoidance syndrome: A necessary distinction within the pervasive developmental disorders. Archives of Disease in Childhood, 88, 595–600.
OCD-UK. (2020). Diagnosing OCD (Online information page). Retrieved from: https://www.ocduk.org/ocd/diagnosing-ocd/ (Accessed 16 January 2021).
O’Nions, E. (2019). Child behaviour and parenting strategies – a research update (Online resource). Retrieved from: https://lizonions.files.wordpress.com/2019/09/1909childbehaviourparentingstrategiessummary.pdf (Accessed 16 January 2021).
O’Nions, E., Christie, P., Gould, J., Viding, E., & Happé, F. (2014). Development of the ‘Extreme Demand Avoidance Questionnaire’ (EDA-Q): preliminary observations on a trait measure for Pathological Demand Avoidance. Journal of Child Psychology and Psychiatry, 55(7), 758–768.
O’Nions, E., Quinlan, E., Caceres, A., Tulip, H., Viding, E., & Happé, F. (2015). Pathological Demand Avoidance (PDA): an examination of the behavioural features using a semi-structured interview (Unpublished research). Retrieved from: http://pdaresource.com/files/An%20examination%20of%20the%20behavioural%20features%20associated%20with%20PDA%20using%20a%20semi-structured%20interview%20-%20Dr%20E%20O’Nions.pdf (Accessed 17 January 2021).
O’Nions, E., Gould, J., Christie, P., Gillberg, C., Viding, E., & Happé, F. (2016a). Identifying features of ‘pathological demand avoidance’ using the Diagnostic Interview for Social and Communication Disorders (DISCO). European Child & Adolescent Psychiatry, 25(4), 407–419.
O’Nions, E., Happé, F., & Viding, E. (2016b). Extreme/’pathological’ demand avoidance. British Psychological Society DECP Debate, Issue 160.
O’Nions, E., Viding, E., Floyd, C., Quinlan, E., Pidgeon, C., Gould, J., & Happé, F. (2018a). Dimensions of difficulty in children reported to have an autism spectrum diagnosis and features of extreme/‘pathological’ demand avoidance. Child and Adolescent Mental Health, 23(3), 220–227.
O’Nions, E., Happé, F., Viding E., Gould, J., & Neons, I. (2018). Demand avoidance is not necessarily defiance. Lancet Child & Adolescent Health, 2(14), e14.
PDA Society. (2020). What is PDA? Booklet (Online booklet). Retrieved from: https://www.pdasociety.org.uk/wp-content/uploads/2020/07/What-is-PDA-booklet-website-v1.1.pdf (Accessed 19 March 2021).
Pellicano, E. (2020). Commentary: Broadening the research remit of participatory methods in autism science – a commentary on Happé and Frith (2020). Journal of Child Psychology and Psychiatry, 61(3), 233–235.
Reilly, C., Atkinson, P., Menlove, L., Gillberg, C., O’Nions, E., Happé, F., & Neville, B. (2014). Pathological Demand Avoidance in a population-based cohort of children with epilepsy: Four case studies. Research in Developmental Disabilities, 35: 3236–3244.
Rosen, N., Lord, C., & Volkmar, F. (2021). The Diagnosis of Autism: From Kanner to DSM‑III to DSM‑5 and Beyond. Journal of Autism and Developmental Disorders. DOI: https://link.springer.com/article/10.1007/s10803-021-04904-1
Rumball, F., Brook, L., Happé, F., & Karl, A. (2021). Heightened risk of posttraumatic stress disorder in adults with autism spectrum disorder: The role of cumulative trauma and memory deficits. Research in Developmental Disabilities, 110(2021), 103848.
Russell, S. (2018). Being Misunderstood: Experiences of the Pathological Demand Avoidance Profile of ASD (Online Report). Retrieved from: https://www.pdasociety.org.uk/resources/2018-summary/ (Accessed 16 January 2021).
Soppitt, R. (2021). Pathological/ Extreme Demand Avoidance (PDA/ EDA). In: Peer, L., & Reid, G (Eds.), Special Educational Needs: A Guide for Inclusive Practice (pp. 296-314). London, Sage Publications Limited.
Stuart, L., Grahame, V., Honey, E., & Freeston, M. (2019). Intolerance of uncertainty and anxiety as explanatory frameworks for extreme demand avoidance in children and adolescents. Child and Adolescent Mental Health, 25(2), 59-67.
Summerhill, L., & Collett, K. (2018). Developing a multi-agency assessment pathway for children and young people thought to have a Pathological Demand Avoidance profile. Good Autism Practice, 19(2), 25–32
Wing, L. (2002). The Autistic Spectrum: A guide for parents and professionals. London: Constable & Robinson Limited.
Wing, L., Gould, J., & Gillberg, C. (2011). Autism spectrum disorders in the DSM-V: Better or worse than the DSM-IV? Research in Developmental Disabilities, 32(2011), 768-773.
Woods, R. (2017). Pathological demand avoidance: my thoughts on looping effects and commodification of autism. Disability & Society, 34(5), 753–758.
Woods, R. (2019a). The PDA paradox: the highs and lows of my life on a little-known part of the autism spectrum. Good Autism Practice, 20(1), 94-95.
Woods, R. (2019b). Demand avoidance phenomena: circularity, integrity and validity – A commentary on the 2018 National Autistic Society PDA Conference. Good Autism Practice, 20(2), 28–40.
Woods, R. (2019c). Is the concept of Demand Avoidance Phenomena (Pathological Demand Avoidance) real or mythical? (Conference paper). Retrieved from: https://www.researchgate.net/publication/340279248_Is_the_concept_of_Demand_Avoidance_Phenomena_Pathological_Demand_Avoidance_real_or_mythical (Accessed 16 January 2021).
Woods, R. (2020a). Commentary: Demand Avoidance Phenomena a manifold issue? Intolerance of uncertainty and anxiety as explanatory frameworks for extreme demand avoidance in children and adolescents: a commentary on Stuart et al (2019). Child and Adolescent Mental Health, 25(2), 68-70.
Woods, R. (2020b). Pathological Demand Avoidance and the DSM-5: a rebuttal to Judy Eaton’s response. Good Autism Practice, 21(2), 74-76.
3 Comments